Epidemiology of Expanding Water Bead Ingestion
Expanding water beads are small, colorful, superabsorbent polymer (SAP) products marketed as sensory toys, decorative items, and gel projectiles for toy guns. Between 2007 and 2022, an estimated 8,159 emergency department (ED) visits in the U.S. involved water bead-related injuries, with children under 5 years old accounting for 55% of cases.
Key Statistics:
Ingestion is the most common mechanism (45.9%).
Injuries also include ear canal insertion (32.6%), nasal insertion (11.7%), and eye trauma (8.8%).
Ingestions were most frequent among 1-year-olds (28.4%) and 2-year-olds (23.4%).
When beads expand to ≥25 mm, surpassing the diameter of the pylorus and small intestine, severe complications like bowel obstruction often occur.
Despite recalls and safety regulations, incidents surged 130.9% from 2021 to 2022, underscoring the need for stricter regulatory measures and caregiver education.
Pharmacokinetics of Water Beads
SAPs do not undergo metabolism, excretion, or absorption. They are inert but can expand in liquid environments, causing physical blockages.
Mechanisms of Toxicity of Water Beads
The toxicity of superabsorbent polymer (SAP) beads arises from their physical, rather than chemical, properties. The primary mechanisms of harm include the following:
Expansion Risk
Depending on the fluid and environmental conditions, SAP beads are designed to absorb liquid and expand dramatically, often up to 300 times their original size. Once ingested, the beads come into contact with gastrointestinal (GI) fluids and absorb them, leading to significant swelling. This expansion can occur over several hours to days, depending on the bead composition and fluid availability, making timely detection and intervention critical.GI Effects of Water Beads
The swollen beads can exert pressure on the walls of the gastrointestinal tract, resulting in:Mechanical obstruction: Large beads or accumulations of multiple beads can block the GI lumen.
Compression ischemia: The pressure created by expanding beads may reduce blood flow to affected areas, potentially damaging tissue.
Perforation: Prolonged compression and ischemia can compromise the integrity of the intestinal wall, causing perforations and increasing the risk of severe infections such as peritonitis.
Obstruction typically occurs in the small intestine, particularly in the duodenum or ileum, where the bowel diameter is narrower and more susceptible to blockage by expanding beads.
High-Risk Groups
Children under 4 years old are at the highest risk due to their smaller bowel size and developmental tendencies to explore objects orally.
Younger children are also more likely to mistake the beads’ candy-like appearance for edible items.
Other Mechanisms
Delayed symptoms: Symptoms such as vomiting, abdominal pain, and constipation may not appear immediately due to the time required for beads to expand, complicating early diagnosis.
Bezoar formation: In some cases, multiple beads may adhere together or form a gelatinous mass, further complicating passage through the bowel.
Secondary Risks
Radiolucency: SAP beads do not appear on standard X-rays, challenging early diagnosis and localization. Imaging modalities like ultrasound or CT scan are more effective.
Aspiration Risk: Rare cases have been reported where beads were aspirated, leading to respiratory complications.
These mechanisms highlight the need for early detection, careful monitoring, and swift management, particularly in high-risk pediatric populations.
Toxic Dose of Water Beads
The risk associated with superabsorbent polymer (SAP) bead ingestion depends on their size, expansion potential, and the environment in which they are exposed. Key considerations include the following:
High-Risk Size Threshold
SAP beads that expand to a hydrated diameter of ≥25 mm are considered to be at high risk of causing gastrointestinal (GI) obstruction.
This size typically exceeds the diameter of the pylorus and small bowel lumen in young children, leading to blockages.
Small Beads and Expansion Potential
When exposed to water or other fluids, beads as small as 2 mm in dry form can grow to 13 mm or more.
Larger beads, such as those starting at 10 mm, can expand to 50 mm, posing a severe obstruction hazard.
Environmental Factors Affecting Expansion
Fluid type: Beads expand more rapidly in water and milk than in simulated gastric fluid, where minimal expansion may occur even after prolonged exposure. However, beads that pass from the stomach to the small intestine can absorb liquids and expand further.
Multiple beads: Ingestion of multiple beads increases the risk of obstruction, as they can form gelatinous masses (bezoars) in the GI tract.
Age and GI Anatomy Considerations
Children under 4 years old are at greater risk as their smaller GI tract diameters can less accommodate expanding beads.
Beads that might pass through the GI tract of older children or adults can cause significant complications in younger patients.
Other Dimensions of Risk
Beads labeled as "safe" due to smaller maximum expansion sizes may still pose a risk if multiple beads are ingested or if the expansion limits exceed safety standards (e.g., 20 mm set by ASTM F963).
Hydrated beads marketed as toys or decorations but exceeding safety thresholds may require regulatory attention to reduce risks.
Even small SAP beads can cause significant harm due to their expansion potential, making any bead capable of swelling beyond 25 mm a serious ingestion hazard. Recognizing the toxic dose threshold is critical for timely intervention and effective management.
Sources of Water Beads
SAP Beads Marketed as Toys
Examples: Popular brands such as Orbeez, Water Balz, and similar products are widely marketed as sensory toys for children. These beads are often brightly colored and candy-like, increasing their appeal to young children.
Marketing Strategies: These products are often advertised for their "fun" properties, such as growing dramatically in size when placed in water, which may encourage children to handle and potentially ingest them.
Decorative Products
Uses: SAP beads are also sold for decorative purposes, including vase fillers, floral arrangement aids, or home decor items.
Risks: Despite being marketed to adults, children can easily access these products in household environments. Their scattered, small, and colorful appearance increases the likelihood of ingestion.
Other Applications
Gel Projectiles for Toy Guns (Gel Blasters): SAP beads are increasingly used as ammunition for toy guns, posing risks not only for ingestion but also for blunt trauma to the eyes.
Agricultural and Gardening Products: Initially developed to retain soil moisture, SAP beads are also used in gardening supplies. However, they are less likely to be ingested than their toy and decorative counterparts.
Unlabeled or Unregulated Products
Beads marketed online or through third-party sellers may lack appropriate labeling, safety warnings, or size limitations, increasing the risk of unsafe use.
Some products are sold in bulk, further increasing the likelihood of unintentional ingestion by children.
The wide-ranging applications of SAP beads across industries, combined with their attractive appearance and accessibility, highlight the importance of vigilance in homes, schools, and recreational settings. Regulatory oversight and caregiver education are essential to reducing risks associated with these sources.
Clinical Presentation and Signs and Symptoms of Water Beads Ingestion Based on Severity
The clinical presentation of superabsorbent polymer (SAP) bead ingestion varies depending on the extent of bead expansion, the location of the obstruction, and the severity of associated complications. Symptoms may develop hours to days after ingestion, making timely recognition critical.
Mild Symptoms of Water Beads ingestion
Asymptomatic: Many cases involve no immediate symptoms, particularly if the bead is small or has yet to expand significantly.
Mild abdominal pain or bloating may result from partial obstruction or early stages of bead expansion.
Moderate Symptoms of Water Beads ingestion
Persistent vomiting: A common sign of obstruction in the upper gastrointestinal tract, such as the duodenum.
Abdominal pain: Pain is localized to the site of obstruction and may intensify with continued bead expansion.
Altered bowel movements:
Constipation: Due to complete or partial obstruction.
Diarrhea May occur proximally to the obstruction as a paradoxical symptom
Severe Symptoms of Water Beads Ingestion
Severe abdominal distension: Results from intestinal blockage and accumulation of fluids and gas.
Signs of obstruction or perforation:
Fever: Suggestive of secondary infection or peritonitis.
Tachycardia and hypotension Indicate systemic involvement and possible sepsis due to perforation.
Severe pain: Associated with ischemia or bowel rupture.
Delayed complications of Water Beads ingestion:
Symptoms such as peritonitis may develop if the obstruction progresses to bowel perforation.
Key Considerations
Younger children (under 4 years old) may present with nonspecific symptoms, such as irritability, refusal to eat, or lethargy, which can delay diagnosis.
Bead location and size and the presence of multiple beads can significantly influence symptom severity.
Radiolucency of beads complicates diagnosis, necessitating reliance on ultrasound or CT imaging for confirmation.
The symptoms of SAP bead ingestion vary widely and may mimic other common pediatric conditions, such as gastroenteritis or constipation. Prompt clinical evaluation is crucial for timely diagnosis and effective management, particularly in symptomatic young children.
Management of Water Beads ingestion Based on Severity
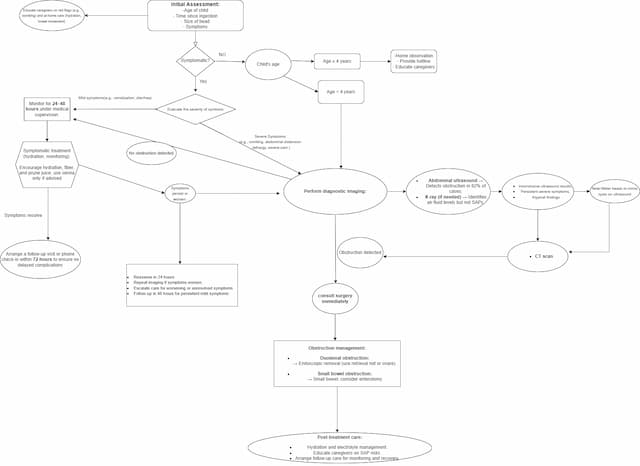
Initial Assessment
A structured evaluation is critical to determine the severity of symptoms and appropriate management:
Key Considerations:
Child's age: Younger children (<4 years) are at higher risk due to smaller bowel size.
Bead size and number: Larger or ingesting multiple beads increases the risk of obstruction.
Symptom onset and progression: Identify early signs of obstruction or perforation.
Risk Stratification for Asymptomatic Cases:
Children ≥4 years:
Safe for home observation with hotline access for symptom monitoring.
Children <4 years:
Recommend early imaging (e.g., ultrasound) to rule out complications.
Diagnostic Imaging for Water Beads Ingestion
Accurate imaging is essential to detect bead presence and complications:
Abdominal ultrasound (preferred): High sensitivity (82%) for detecting obstructions or bead presence in the GI tract.
CT scan: Useful for inconclusive ultrasound findings or to evaluate complications such as perforation.
X-ray: Identifies air-fluid levels associated with obstruction but cannot directly visualize SAP beads due to their radiolucent nature.
Management Based on Severity
Mild Symptoms
Children ≥4 years:
Monitor at home: Provide education on warning signs such as vomiting, abdominal pain, or changes in bowel movements.
Children <4 years:
Perform early imaging to rule out obstruction.
Observe in a medical setting for 24–48 hours to monitor for delayed symptom development.
Moderate Symptoms
Hospital Admission:
Provide hydration and electrolyte management to maintain homeostasis.
Conduct diagnostic imaging to confirm the presence and location of obstructions.
Monitoring:
Observe closely for worsening symptoms, such as increased abdominal pain, distension, or systemic signs like fever.
Severe Symptoms
Confirmed Obstruction:
Duodenal obstruction: Perform endoscopic removal using a retrieval net or polyp snare to safely extract the beads.
Small bowel obstruction: Surgical intervention (e.g., enterotomy) may be required for bead removal.
Supportive Care:
Administer IV fluids to address dehydration and electrolyte imbalances.
Start broad-spectrum antibiotics if perforation or sepsis is suspected.
Provide pain management as needed.
The management of SAP bead ingestion depends on symptom severity and patient age. Early assessment and imaging are key to identifying complications and preventing severe outcomes. Tailored interventions, from observation to surgical removal, ensure effective and safe treatment.
Post-Treatment Care
Reassess symptoms within 24–48 hours if obstruction is ruled out.
Educate caregivers about the risks of SAP ingestion.
Arrange follow-up care for full recovery.
Antidote
There is no antidote available. GI decontamination (e.g., whole bowel irrigation) is contraindicated due to the risk of increased swelling.
Observation Criteria
Children
Asymptomatic Children (≥4 Years Old):
Safe for home monitoring with caregiver education on:
Recognizing warning signs such as vomiting, abdominal pain, and changes in bowel movements.
Access a poison control hotline or healthcare provider for guidance if symptoms develop.
Symptomatic or High-Risk Cases (Children <4 Years Old):
Require hospital observation for 24–48 hours to monitor for:
Delayed symptom onset or worsening of existing symptoms.
Complications such as obstruction or perforation.
Frequent reassessment by clinical staff is necessary to identify progression early.
Adults
Rarely Affected:
Cases are uncommon due to larger GI tract size and reduced risk of obstruction.
If symptoms arise (e.g., obstruction), manage with:
Imaging will confirm the location of the obstruction.
Endoscopic or surgical removal as necessary.
Key Notes for Caregivers and Clinicians
Education for caregivers is critical in preventing re-exposure and recognizing symptoms in asymptomatic cases managed at home.
In hospital settings, timely imaging and clinical monitoring are pivotal for high-risk groups.
Adults presenting with symptoms require individualized evaluation based on imaging results and symptom severity.
Age, symptomatology, and risk stratification guide observation criteria. Adherence to these guidelines ensures effective monitoring while minimizing unnecessary hospital admissions.
Prevention and Public Health Measures
Prevention strategies focus on reducing the risk of ingestion and complications associated with superabsorbent polymer (SAP) beads. These measures target caregivers, healthcare providers, and policymakers to create safer environments for children.
Raise Awareness of SAP Bead Risks Among Caregivers
Education campaigns: Inform caregivers about the potential dangers of SAP beads, particularly their ability to expand dramatically and cause severe gastrointestinal complications.
Safe storage practices: Encourage caregivers to store SAP beads out of the reach of children, especially in households with children under 4 years old.
Highlight the visual resemblance of beads to candy, emphasizing the need for vigilance in preventing access.
Advocate for Stricter Regulations on SAP Toy Sales and Labeling
Product design standards: Promote the development of SAP beads with reduced expansion capacity to minimize mechanical risks.
Stronger safety labeling: Clear warnings on packaging are required about the risks of ingestion and potential for obstruction, especially for products marketed as toys or sensory tools.
Age restrictions: Enforce stricter age recommendations for SAP bead products, disallowing their sale for use by children under 4 years old.
Regulatory enforcement: Advocate for compliance with international safety standards (e.g., ASTM F963) and support enacting stricter laws, such as the proposed Esther’s Law in the U.S., to limit bead expansion and enforce broader marketing restrictions.
Educate Pediatricians and Caregivers on Early Signs of Complications
Healthcare provider training: Equip pediatricians, family physicians, and emergency department staff with knowledge on identifying and managing SAP bead-related injuries.
Symptom awareness: Educate caregivers on recognizing early warning signs of bead ingestion, such as vomiting, abdominal pain, or changes in bowel movements, and the need for prompt medical evaluation.
Collaborate with Retailers and Manufacturers
Encourage retailers to discontinue sales of high-risk SAP beads, as has been done by some major U.S. retailers, such as Walmart, Amazon, and Target.
Advocate for developing safer alternatives, such as non-expanding sensory beads or toys designed with safety in mind.
Community and School Outreach
Partner with schools, childcare centers, and parenting groups to distribute educational materials and promote safe practices.
Develop age-appropriate educational programs for children to recognize and avoid unsafe objects.
Conclusion
Preventing SAP bead-related injuries requires a multifaceted approach, combining caregiver education, regulatory action, and healthcare provider involvement. Collaborative efforts between public health agencies, manufacturers, and communities can significantly reduce the risks of SAP bead use.
