Epidemiology of Substance Poisoning (Updated)
Local anesthetics are frequent pharmaceutical exposures; lidocaine is among the most reported.
Serious outcomes are uncommon but cluster with infant/child ingestions, large intentional overdoses, or repeated/stacked dosing.
The FDA (2014) warns against using 2% viscous lidocaine for infant teething due to seizures, severe CNS depression, and deaths after small volumes.
Pharmacokinetics
Absorption and Peak Concentration
Rapid oropharyngeal/mucosal absorption (partly bypasses first-pass metabolism).
GI absorption is variable; Tmax ~30–60 min after ingestion; mucosal effects can start in 15–30 min.
Oropharyngeal anesthesia transiently increases aspiration risk.
Metabolism
Hepatic (CYP1A2, CYP3A4) → active metabolites MEGX (monoethylglycinexylidide) and GX (glycinexylidide).
Half-Life
Adults: ~1.5–2 h (prolonged with hepatic disease/heart failure).
Neonates/infants: longer (~3–5+ h).
Excretion
Renal as metabolites; <10% excreted unchanged.
Bioavailability
Oral ≈ 35% (first-pass). Mucosal absorption can produce higher, faster systemic exposure.
Mechanisms of Toxicity
Voltage-gated sodium channel blockade → CNS excitation (tinnitus, perioral numbness, metallic taste) → CNS depression (seizures, coma).
Cardiac: conduction slowing (PR/QRS prolongation), myocardial depression, ventricular dysrhythmias, hypotension (vasodilation + negative inotropy).
Methemoglobinemia: very rare with lidocaine (far more common with benzocaine/prilocaine) but possible at high doses.
Risk amplified by acidosis, hypercarbia, hypoxia, low α1-acid glycoprotein (infants), and CYP inhibitors.
Toxic Dose (Triage Thresholds for ED Referral)
2% = 20 mg/mL • 5 mL (1 tsp) = 100 mg • 15 mL (1 Tbsp) = 300 mg
Quick check: mg/kg = 20 × mL ingested ÷ weight (kg)
Refer to ED if ≥ any of the following (these are conservative triage cutoffs, not toxicity guarantees):
Infants (<12 months): ≥1.5 mg/kg (≈ 0.075 mL/kg) or any non-therapeutic exposure.
Children: ≥3 mg/kg (≈ 0.15 mL/kg) or any symptoms.
Adults: ≥4.5 mg/kg (≈ 0.225 mL/kg), unknown amount, or any symptoms.
Examples
10-kg toddler @ 3 mg/kg → 30 mg ≈ 1.5 mL
20-kg child @ 3 mg/kg → 60 mg ≈ 3 mL
70-kg adult @ 4.5 mg/kg → 315 mg ≈ 16 mL
Higher risk at lower doses with: hepatic/cardiac disease, pregnancy, low body mass, CYP inhibitors (e.g., amiodarone, cimetidine, clarithromycin, fluoxetine, itraconazole, verapamil), or co-exposure to other local anesthetics.
Sources
Prescription 2% viscous lidocaine (mouth/throat/esophageal analgesia).
Other forms: dermal gels/sprays/patches, dental preparations, infiltration/nerve block solutions, IV antiarrhythmic (additive exposure risk).
Therapeutic and Toxic Serum Concentrations
Therapeutic (antiarrhythmic): 1.5–5 µg/mL (mg/L)
Early neurotoxicity: >5 µg/mL
Seizures: ~8–12 µg/mL
Severe cardiotoxicity/collapse: >20 µg/mL
Levels are rarely timely and do not guide initial triage/management.
Clinical Presentation and Signs & Symptoms
Mild
Perioral/tongue numbness, metallic taste, tinnitus, dizziness, visual blurring, nausea/vomiting, mild anxiety/drowsiness.
Oropharyngeal anesthesia → aspiration risk.
Moderate
Agitation, confusion, tremor, seizure, ataxia.
Vitals: hypotension or tachycardia. ECG: PR/QRS prolongation, AV block.
Severe
Refractory seizures/status epilepticus, coma.
Ventricular dysrhythmias, profound hypotension, bradycardia/asystole, cardiovascular collapse.
Methemoglobinemia (rare): cyanosis with normal PaO₂, chocolate-colored blood, low pulse oximetry unresponsive to O₂.
Infants may present without a classic excitation prodrome—apnea or seizure can be the first sign.
Management of Toxicity (By Severity)
Immediate Priorities (all patients)
ABCs, high-flow oxygen, IV access, continuous ECG + pulse oximetry; consider capnography.
Check glucose early; correct hypoglycemia.
NPO until gag returns (≈ 60 min after oropharyngeal anesthesia).
Decontamination: No emesis. Activated charcoal only for large, early (<1–2 h) ingestions if airway is protected (intubated) due to aspiration risk.
Conduction delay & acidosis
Optimize ventilation to correct hypercarbia/acidosis.
If marked QRS widening from Na⁺ channel blockade, consider sodium bicarbonate 1–2 mEq/kg IV (bolus), especially with associated acidosis.
Mild
Cardiac monitoring; antiemetics as needed.
If asymptomatic after a small exposure: observe 4–6 h (children ≥6 h).
Moderate
Seizures: Benzodiazepines first-line
Adults: lorazepam 0.1 mg/kg IV (max 4 mg) or diazepam 0.15–0.2 mg/kg IV.
Children: lorazepam 0.1 mg/kg IV (max 4 mg) or midazolam 0.1 mg/kg IV/IM.
Avoid phenytoin/fosphenytoin (Na⁺ channel blockers) in LAST.
Hypotension: isotonic fluids → small epinephrine boluses (10–100 µg IV) if needed.
Avoid vasopressin and avoid additional local anesthetics (e.g., do not use lidocaine as an antiarrhythmic).
Severe (LAST – Local Anesthetic Systemic Toxicity)
20% Intravenous Lipid Emulsion (ILE) – initiate early
Bolus: 1.5 mL/kg IV over ~1 min.
Infusion: 0.25 mL/kg/min.
If instability persists: repeat 1.5 mL/kg bolus up to 2–3× and increase infusion to 0.5 mL/kg/min.
Continue infusion ≥10 min after hemodynamic stability.
Upper limit: about 10–12 mL/kg in the first 30 min.
ACLS with LAST modifications
Prefer amiodarone for ventricular dysrhythmias.
Keep epinephrine doses small; avoid vasopressin.
Avoid large doses of propofol in hemodynamically unstable patients.
Airway control early for recurrent seizures/AMS (consider non-depolarizing NMBs if needed).
Methemoglobinemia: Methylene blue 1–2 mg/kg IV over 5 min; may repeat once at 30–60 min. Use caution in G6PD deficiency.
Hemodialysis is not useful (large Vd, protein binding, lipophilicity).
Post-ILE caveat: lipemia may interfere with some lab assays and extracorporeal circuits.
Antidote
20% Intravenous Lipid Emulsion is the preferred “antidotal” therapy for severe LAST.
Methylene blue is the antidote for clinically significant methemoglobinemia.
Observation Criteria
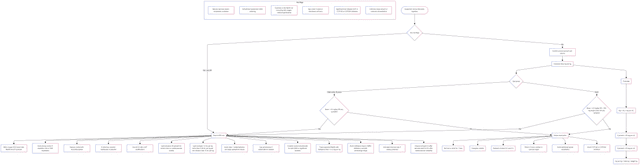
Children
ED referral: any symptoms; any infant exposure beyond prescribed use; or ≥3 mg/kg (≈ 0.15 mL/kg of 2%).
Monitoring: ≥6 h after last symptom; longer for large doses, hepatic disease, or interacting meds.
Discharge: asymptomatic with normal ECG for ≥6 h and reliable caregivers.
Adults
Home observation (with poison center guidance) may be acceptable if asymptomatic, <4.5 mg/kg by reliable history (e.g., <15–16 mL for a 70-kg adult), no risk factors/interactions, and ready access to care.
ED referral: any symptoms, large/unknown amount, hepatic/cardiac disease, pregnancy, significant CYP inhibitors, or co-exposures to other local anesthetics.
Monitoring: 4–6 h if asymptomatic; ≥6–8 h if symptomatic/high-risk; longer if ILE given.
Prevention and Public Health Measures
Do not use viscous lidocaine for infant teething.
Store in child-resistant containers; avoid bedside storage.
Use measuring devices; avoid “sips/swigs”.
Prefer swish-and-spit when appropriate; if swallowing is prescribed (e.g., esophageal pain), enforce strict dose limits and spacing (no redosing for several hours).
Avoid eating/drinking for ~60 min after oropharyngeal application.
Screen for CYP interactions; avoid stacking multiple local anesthetics.
References:
References :
Neal JM, Barrington MJ, Fettiplace MR, Rubin DS, Weinberg GL, et al. The third American Society of Regional Anesthesia and Pain Medicine Practice Advisory on local anesthetic systemic toxicity. Reg Anesth Pain Med. 2018;43(2).
Neal JM, Mulroy MF, Weinberg GL. The American Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity. Reg Anesth Pain Med. 2012;37(1).
Nelson LS, Howland MA, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS, editors. Goldfrank’s Toxicologic Emergencies. 11th ed. New York: McGraw-Hill Education; 2019.
