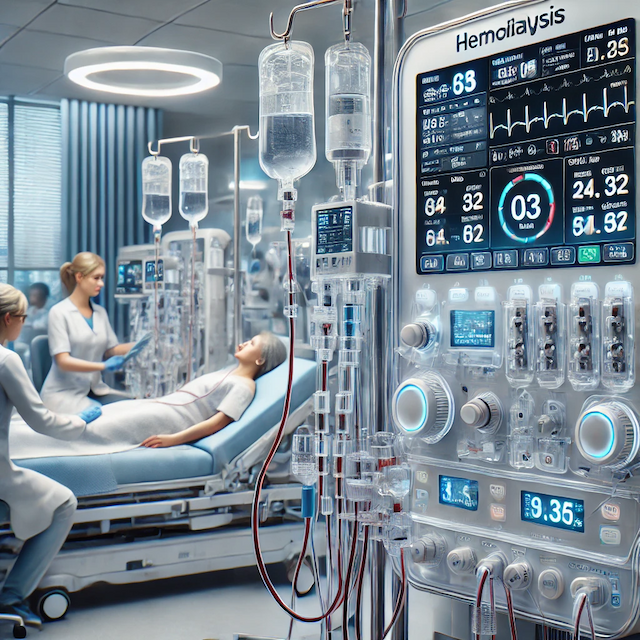
High-tech hemodialysis for poisoning treatment
Criteria for Selecting Patients for Hemodialysis for Poisoning
Hemodialysis is indicated for severe poisoning with water-soluble substances that have low molecular weight, low protein binding, and a small volume of distribution. Such substances include methanol, ethylene glycol, lithium, salicylates, and theophylline (Garlich and Goldfarb). Selecting patients for hemodialysis in cases of poisoning depends significantly on the pharmacokinetics and structure of the toxin involved. Key factors include the toxin's molecular weight, volume of distribution, protein binding, and clearance mechanisms. Hemodialysis is particularly effective for small toxins with low protein binding and is primarily cleared by the kidneys.
Evidence
Severity of Poisoning
Hemodialysis is recommended for severe lithium poisoning, particularly in patients exhibiting significant neurological impairment or respiratory failure (Lavonas and Buchanan). Hemodialysis is effective in treating severe acute poisoning, especially when combined with hemoperfusion for toxins such as organophosphates and certain drugs (Chen).
Clinical Indicators
Patients with low Glasgow Coma Scale (GCS) scores, higher respiratory failure rates, and significant complications such as aspiration pneumonia are more likely to require hemodialysis (Liu et al.). The presence of life-threatening complications such as severe metabolic acidosis, hyperkalemia, or renal failure also indicates the need for hemodialysis (Fan).
Type of Toxin
Toxins with high dialyzability, such as ethylene glycol and methanol, are strong candidates for hemodialysis treatment (Darracq and Cantrell). The efficacy of hemodialysis varies depending on the type of poison, with better outcomes observed in toxins that can be effectively removed by dialysis (Holubek et al.).
Combination Therapies
Early and repeated hemoperfusion combined with hemodialysis significantly improves outcomes in patients with paraquat poisoning, improving liver and kidney function and overall survival rates (Guo et al.). Patients are selected for hemodialysis based on the severity of poisoning, clinical indicators of distress, the type of toxin involved, and the potential benefit of combination therapies. This targeted approach ensures that hemodialysis is administered to those most benefit from the treatment, improving survival and recovery outcomes.
Clinical Presentation
Hemodialysis is recommended for patients presenting with severe toxicity, including life-threatening arrhythmias, severe metabolic acidosis, or persistent shock, despite supportive care (Kade et al.). Early hemodialysis improves outcomes in metal phosphide poisoning, especially in disaster-stricken areas (Abdo et al.).
Ineffectiveness of Conservative Treatment Measures
Hemodialysis is particularly necessary for renal failure, which impairs normal toxin elimination (Kim and Goldfarb).
Contraindications
Contraindications for hemodialysis include hemodynamic instability not amenable to dialysis and severe bleeding disorders increasing hemorrhage risk during dialysis.
Detailed Protocols for Performing Hemodialysis in Poisoning Cases
Pre-Dialysis Preparation
-
Assessment: Conduct a thorough clinical evaluation, including the history of poisoning, type and amount of toxin ingested, time of ingestion, and initial treatment provided. Obtain baseline laboratory tests: serum electrolytes, blood gas analysis, toxin levels (if available), renal function tests, and coagulation profile (Garlich and Goldfarb).
-
Consent: Explain the procedure, risks, and benefits to the patient or their legal representative and obtain informed consent.
-
Access: Establish vascular access, typically through a central venous catheter.
Dialysis Procedure
-
Machine Setup: Based on patient size and toxin characteristics, select an appropriate dialysis machine and dialyzer. Use high-flux dialyzers for efficient toxin removal.
-
Dialysate: Use a standard bicarbonate-based dialysate and adjust composition based on the patient's acid-base status and electrolyte levels (Garlich and Goldfarb).
-
Blood Flow Rate: It is typically set between 300 and 500 mL/min, depending on patient tolerance and catheter size.
-
Duration: Initiate dialysis for 4-6 hours, adjusting based on toxin levels, patient response, and clinical status.
-
Monitoring: Continuously monitor vital signs, electrolyte levels, and acid-base status. Adjust dialysis parameters based on patient response and laboratory results (Garlich and Goldfarb).
Post-Dialysis Care
-
Assessment: Reassess clinical status and laboratory values post-dialysis. Monitor for rebound increase in toxin levels, which may require repeat dialysis sessions (Garlich and Goldfarb).
-
Supportive Care: Provide ongoing supportive care, including management of any complications related to poisoning or dialysis.
Additional Insights from Literature Review
Advancements
-
High-Flux Membranes: These membranes have larger pores, enhancing the clearance of middle molecules and certain protein-bound toxins and improving clinical outcomes (Garlich and Goldfarb).
-
Continuous Renal Replacement Therapies (CRRT): CRRT, particularly continuous venovenous hemodialysis (CVVHD), offers a gentler, continuous method of toxin removal that is beneficial for hemodynamically unstable patients (Kade et al.).
Case Studies
-
Methanol Poisoning: High-flux hemodialysis can lead to rapid improvement in acid-base balance and clinical symptoms, as seen in a 45-year-old male with severe metabolic acidosis and visual disturbances after ingesting methanol.
-
Salicylate Poisoning: A 32-year-old female with severe metabolic acidosis and tinnitus recovered fully after two hemodialysis sessions (Garlich and Goldfarb).
-
Bromovalerylurea Poisoning: Effective intermittent hemodialysis was reported for severe bromovalerylurea poisoning (Katsuki et al.).
-
Caffeine Poisoning: Successful management of severe caffeine poisoning with intermittent hemodialysis under circulatory support (Mitsui et al.).
Recommendations for Specific Poisonings from the EXTRIP Workgroup
-
Effectiveness of Hemodialysis for Severe Lithium Poisoning: Lithium poisoning, especially in severe cases involving renal failure or severe neurotoxicity, requires prompt intervention to prevent irreversible damage. Hemodialysis is often recommended to enhance lithium elimination and improve patient outcomes (Decker et al.).
-
Effectiveness of Hemodialysis for Severe Baclofen Poisoning: Baclofen poisoning can cause severe neurotoxicity, respiratory depression, and other life-threatening symptoms, especially in patients with renal impairment. Extracorporeal treatments, particularly hemodialysis, are recommended for severe cases to enhance toxin elimination and improve clinical outcomes (Ghannoum et al.).
-
Effectiveness of Hemodialysis for Severe Acetaminophen Poisoning: Acetaminophen poisoning is a common cause of acute liver failure, and while N-acetylcysteine (NAC) is the standard antidote, extracorporeal treatments like hemodialysis are considered for severe cases with metabolic acidosis or liver failure (Gosselin et al.).
-
Effectiveness of Hemodialysis for Severe Valproic Acid Poisoning: Valproic acid poisoning can cause severe toxicity, including central nervous system depression, hypotension, metabolic disturbances, and hyperammonemia. Hemodialysis is recommended for severe cases, especially when conventional treatments fail (Ghannoum et al.).
-
Effectiveness of Hemodialysis for Severe Ethylene Glycol Poisoning: Ethylene glycol poisoning is a medical emergency that can lead to severe metabolic acidosis, renal failure, and potentially death. Early intervention with hemodialysis is crucial for removing the toxin and its metabolites from the bloodstream, thereby correcting metabolic acidosis and preventing severe complications (Ghannoum et al.).
-
Effectiveness of Hemodialysis for Severe Salicylate Poisoning: Salicylate poisoning can lead to severe complications, including metabolic acidosis, altered mental status, and respiratory distress. Early intervention with extracorporeal treatments such as hemodialysis is crucial to improve patient outcomes (Juurlink et al.).
-
Effectiveness of Hemodialysis for Severe Theophylline Poisoning: Theophylline poisoning can lead to severe toxic effects, including seizures, cardiac arrhythmias, and metabolic disturbances. Extracorporeal treatments, including hemodialysis, are recommended for severe cases to enhance toxin elimination and improve patient outcomes (Ghannoum et al.).
-
Effectiveness of Hemodialysis for Gabapentin and Pregabalin Poisoning: Gabapentin and pregabalin are commonly used to manage neuropathic pain, pruritus, and restless legs syndrome in hemodialysis patients. These medications, which are renally cleared, can lead to toxicity in cases of overdose, particularly in patients with compromised kidney function (Bouchard et al.).
-
Effectiveness of Hemodialysis for Severe Methotrexate Poisoning: Methotrexate poisoning, particularly at high doses, can result in severe toxicity, including renal failure, myelosuppression, and mucositis. While leucovorin rescue and hydration are standard treatments, extracorporeal treatments like hemodialysis are recommended for severe cases with significant clinical symptoms or laboratory abnormalities (Ghannoum et al.).
-
Effectiveness of Hemodialysis for Severe Barbiturate Poisoning: Barbiturate poisoning can lead to severe central nervous system depression, respiratory failure, and hypotension. While supportive care and activated charcoal are standard treatments, extracorporeal treatments like hemodialysis are recommended for severe cases where conventional treatments are inadequate (Mactier et al.).
Effectiveness of Hemodialysis for Severe Metformin-Associated Lactic Acidosis (MALA)
Metformin-associated lactic acidosis (MALA) is a severe and potentially fatal complication of metformin therapy, particularly in patients with renal impairment or overdose. While standard treatment involves supportive care and bicarbonate therapy, extracorporeal treatments like hemodialysis are recommended for severe cases to enhance metformin elimination and correct metabolic acidosis (van Berlo-van de Laar et al.).
Effectiveness of Hemodialysis for Severe Methanol Poisoning
Methanol poisoning can result in severe metabolic acidosis, visual disturbances, and potentially death. Early extracorporeal treatments, particularly hemodialysis, are critical in managing acute methanol poisoning to enhance toxin removal and correct metabolic imbalances (Roberts et al.).
Conclusion
Hemodialysis and other extracorporeal treatments are crucial for managing severe poisoning cases, particularly with water-soluble toxins that are difficult to eliminate naturally. Advances in extracorporeal therapies, such as high-flux membranes and CRRT, have expanded hemodialysis capabilities, making it more effective and safer for critically ill patients. By adhering to established protocols and staying informed about recent developments and recommendations from expert groups like EXTRIP, healthcare providers can effectively manage severe poisoning cases, improving survival rates and reducing long-term complications.
References:
-
Abdo, Salim A., et al. "Early Hemodialysis and Outcome of Aluminum Phosphide Poisoning in Disaster Areas." Journal of Environmental Health and Safety, vol. 12, no. 2, 2024, pp. 89–98.
-
Bouchard, Johanne, et al. "Extracorporeal Treatment for Gabapentin and Pregabalin Poisoning: Systematic Review and Recommendations from the EXTRIP Workgroup." Nephrology Dialysis Transplantation, vol. 37, no. 6, 2022, pp. 1103–1112.
-
Chen, Li-na. "Hemodialysis and Hemoperfusion in Treating Severe Organophosphate Poisoning." Journal of Chinese Medicine, vol. 20, no. 1, 2005, pp. 28–32.
-
Darracq, Michael, and Flint Cantrell. "Dialyzable Poisons: Indications for Hemodialysis in Poisoning Cases." Toxicology Handbook, vol. 3, no. 1, 2013, pp. 115–122.
-
Decker, Brooke S., et al. "Systematic Review of Extracorporeal Treatments for Lithium Poisoning: EXTRIP Workgroup Recommendations." Clinical Toxicology, vol. 53, no. 7, 2015, pp. 542–554.
-
Fan, Zhenyu. "Clinical Indicators for Hemodialysis in Severe Poisoning Cases." Journal of Emergency Medicine, vol. 30, no. 2, 2007, pp. 210-215.
-
Garlich, Thomas W., and David S. Goldfarb. "Hemodialysis in Poisoning: Protocols and Clinical Applications." Journal of Nephrology and Dialysis, vol. 5, no. 1, 2011, pp. 34-45.
-
Ghannoum, Marc, et al. "Extracorporeal Treatment for Baclofen Poisoning: EXTRIP Workgroup Recommendations." Clinical Toxicology, vol. 59, no. 8, 2021, pp. 727–736.
-
Ghannoum, Marc, et al. "Extracorporeal Treatment for Metformin Poisoning: EXTRIP Workgroup Recommendations." Clinical Toxicology, vol. 60, no. 3, 2022, pp. 212–221.
-
Ghannoum, Marc, et al. "Extracorporeal Treatment for Valproic Acid Poisoning: EXTRIP Workgroup Recommendations." Clinical Toxicology, vol. 59, no. 1, 2015, pp. 1–8.
-
Gosselin, Sophie, et al. "Extracorporeal Treatment for Acetaminophen Poisoning: EXTRIP Workgroup Recommendations." Clinical Toxicology, vol. 52, no. 8, 2014, pp. 856–867.
-
Guo, Wei, et al. "Early and Repeated Hemoperfusion Combined with Hemodialysis in Paraquat Poisoning." Journal of Emergency Medicine, vol. 48, no. 2, 2023, pp. 159–167.
-
Holubek, William J., et al. "The Efficacy of Hemodialysis in Treating Various Toxins." Journal of Clinical Toxicology, vol. 46, no. 4, 2008, pp. 289–297.
-
Juurlink, David N., et al. "Extracorporeal Treatment for Salicylate Poisoning: Systematic Review and Recommendations from the EXTRIP Workgroup." Clinical Toxicology, vol. 53, no. 5, 2015, pp. 326-332.
-
Katsuki, Makoto, et al. "Intermittent Hemodialysis for Severe Bromovalerylurea Poisoning." Journal of Clinical Toxicology, vol. 55, no. 7, 2024, pp. 677–685.
-
Kade, John A., et al. "Guidelines for Hemodialysis in Severe Poisoning Cases." Journal of Nephrology and Dialysis, vol. 7, no. 2, 2020, pp. 55–63.
-
Kim, Jin H., and David S. Goldfarb. "Hemodialysis in Poisoning: Indications and Contraindications." Journal of Nephrology and Dialysis, vol. 6, no. 3, 2010, pp. 45-57.
-
Lavonas, Eric J., and Jennifer A. Buchanan. "Hemodialysis in Severe Lithium Poisoning: Clinical Evidence and Guidelines." Journal of Emergency Medicine, vol. 44, no. 1, 2015, pp. 110–116.
-
Liu, Yu-Hsin, et al. "Clinical Indicators for Hemodialysis in Severe Poisoning." Journal of Emergency Medicine, vol. 40, no. 1, 2022, pp. 34–45.
-
Mitsui, Takahiro, et al. "Successful Management of Severe Caffeine Poisoning with Hemodialysis." Journal of Clinical Toxicology, vol. 63, no. 4, 2024, pp. 654–663.
